This is a viral infectious disease that affects the upper respiratory tract. She is also known as acute viral nasopharyngitis or coryza. Being the most common infectious disease Around the world, colds are mainly caused by coronavirus or rhinovirus.
Causes of Infectious Colds
The human body cannot resist absolutely all viruses that can cause a cold. This is why colds are so common and reoccurring. According to the US Centers for Disease Control and Prevention, children in kindergarten get an average of 12 colds a year, compared with teens and adults, who get about seven colds a year. These are very impressive numbers. It's worth thinking about them.
Colds can be caused by more than 200 different types viruses. Up to 50% colds caused by rhinoviruses that cause other cold viruses:
- Parainfluenza virus
- Metapneumovirus
- Coronavriuses adenovirus
- Respiratory syncytial virus
- Enteroviruses
When the virus manages to overcome the infection, the immune system the body becomes more powerful. The body's first line of defense is mucus, which is produced in the nose and throat (mucus is produced by glands). This mucus makes breathing very difficult. The mucus itself is a slippery liquid that is localized on the membranes of the nose, mouth, throat and vagina. This is the most common cold symptom in cold weather. winter months, which affects children and adults of all ages. Most people get colds two to four times a year.
The incubation period for a cold lasts from 1 to 4 days. The infection is transmitted through airborne droplets when a patient coughs or sneezes. Infection can also be spread by dirty hands by touching your nose or mouth or eyes. This is perhaps the most common way the virus is transmitted. Causing colds.
Symptoms of an Infectious Cold
- A sore throat
- Sore throat when swallowing
- Sneezing
- Mucus during a runny nose initially resembles water, then the mucus secretion gradually becomes thicker and more yellow.
- When the lining of the nose becomes swollen, a person may have difficulty breathing through the nose
- Aching sensation or ringing in the ears
- Headache
- Cough
- Feeling very unwell
- Heat
- Children are more prone to fever than adults.
Preventing Infectious Colds
- If possible, stay away from people with colds.
- Avoid crowded places where the risk of catching a cold is much higher
- Avoid touching your nose or eyes after you have been in physical contact with someone who has a cold.
- Wash your hands thoroughly, especially when you have a runny nose
- Ventilate your room well
Treatment of Infectious Colds
There is no clear answer against colds effective ways treatment to make it go away faster. If the patient has no other illness than a common cold and it goes away in just one to two weeks, there is no reason to see a doctor.
It is worth knowing that if a cold is caused by a virus, antibiotics are not suitable for treatment.
- Make sure you drink plenty of non-alcoholic liquids, ideally purified water - this is especially important for children. Many cold symptoms go away much faster after drinking warm drinks.
- Sleep on a high pillow.
- If you have a cold, there is no need to change your daily activities. But you should know that if you have a cold, you will get tired much faster. Therefore, get plenty of rest. And children with colds also need more rest.
- Avoid smoking. It irritates the nasal mucosa even more.
Nasal congestion and chest cough can be relieved by steam inhalation, which helps loosen these mucus and reduce the symptoms of a runny nose. Sit comfortably and tilt your head over a bowl of hot water, place a towel on your head, close your eyes and inhale the steam deeply. Very effective method getting rid of a runny nose. However, this method is not recommended for children due to the risk of burns.
Symptoms such as cough, sore throat, nasal congestion and headache can be relieved with a variety of nasal remedies and over-the-counter medications that can help make breathing easier. It is advisable to consult your doctor about which medications are most suitable for you and your symptoms.
Colds or acute respiratory infections (ARVI) are large group acute respiratory tract infections, which have a similar mechanism of transmission and development of the disease.
ARI is an abbreviation for “acute respiratory disease” - can be caused by viruses, bacteria and other microorganisms, ARVI is an acute respiratory viral disease. Since in practice it is very difficult to determine what type of pathogen caused the symptoms of a cold, a diagnosis of acute respiratory infections (ARVI) is usually made, and some doctors, given that 90% of all colds are caused by viruses, simply write ARVI.
Cold symptoms are also accompanied by intestinal infections caused by rotavirus (more often in children) and norovirus (in adults).
The cold is a very common illness that usually does not pose a serious health threat and goes away on its own within a week or two. However, during this period and several days before the first symptoms appear, a person is a source of infection for others, so it is advisable to stay at home during illness.
You can get a cold by:
- inhaling tiny droplets of liquid that contain infectious agents - they enter the air when a sick person sneezes or coughs;
- touching objects contaminated with secretions, including the skin of a sick person, with your hands, and then touching your face, mouth, nose or eyes.
Colds spread most easily among people who are in constant close contact, for example, in a family, in a group of children kindergarten or schools. Most outbreaks occur in winter time year, although the reasons for seasonality are not entirely clear.
There are a lot of causative agents of colds, so there are cases of repeated illnesses, when the first acute respiratory infection is followed by another, caused by another infection, etc. The most common causative agents of acute respiratory infections (except influenza) are:
- adenoviruses, enteroviruses, reoviruses, rhinoviruses, coronaviruses, herpes viruses, parainfluenza viruses, respiratory syncytial virus and others;
- bacteria: streptococci, staphylococci, meningococci, Haemophilus influenzae, legionella, pneumococci, etc.
- chlamydia, mycoplasma, as well as the group of the above infectious agents.
The symptoms of a cold may vary depending on the pathogen and individual characteristics organism, but they are all very similar.
Symptoms of a cold (ARD, ARVI)
Symptoms of acute respiratory infections or acute respiratory viral infections usually develop over several days, and not suddenly. The main ones:
- sore throat or hoarseness;
- nasal congestion or discharge from the nasal passages;
- sneezing or coughing;
- general poor health.
Less commonly observed:
- increase in body temperature, usually up to 37-39 oC;
- headache;
- pain in the ear (severe pain in the ear may indicate the addition of otitis media);
- loss of smell and dullness of taste;
- mild eye irritation;
- a feeling of pressure in the ears and face, as a result of inflammation and swelling.
The worst state of health is usually typical for 2-3 days of illness, then the condition begins to slowly improve. In adults and older children, cold symptoms may persist for 7-10 days or slightly longer. For example, a cough can last up to 2-3 weeks.
Colds in children under 5 years of age are characterized by a longer course—the duration of their illness, on average, is 10-14 days.
Cold or flu: how to tell the difference?
It is not always possible to accurately distinguish a common ARVI from the flu, but there are some characteristic features, which can be used to suggest the nature of the cold.
Flu symptoms begin acutely, with signs of illness appearing within a few hours:
- headache, pain in muscles, bones, eyeballs, severe weakness, weakness - signs of intoxication;
- increase in body temperature to 39°C and above;
- rawness deep in the throat, behind the sternum, dry cough - manifestations of tracheitis;
- A runny nose is not typical for influenza at all or appears only on the 2-3rd day of illness.
Symptoms of a common cold usually begin gradually, feeling worse within 1-2 days:
- The first to appear are a runny nose, sneezing, redness and sore throat, which gets worse when swallowing; a cough may appear only on the 2-3rd day;
- the temperature rarely rises to 39°C or higher, usually stays within 37.5-38.5°C or remains normal;
- the general condition suffers to a lesser extent than with the flu.
It is useful to distinguish between a simple acute respiratory infection and the flu because the flu has a more unfavorable prognosis, lasts longer and requires serious treatment.
Treatment of colds (acute respiratory infections, acute respiratory viral infections)
A healthy body usually copes with mild cases of acute respiratory infections on its own, so you can be treated at home using symptomatic remedies (alleviating the course of the disease). However, even with acute respiratory infections, it is advisable to consult a doctor if:
- you require sick leave or a certificate for the child;
- You are pregnant;
- you have severe chronic diseases, for example, heart disease, kidney disease, lung disease;
- a child under 5 years of age or an elderly person falls ill;
- your health does not improve within 3-5 days;
- shortness of breath, chest pain, and coughing up blood appeared.
- try to drink more fluid to replenish its losses (through sweat, nasal discharge, etc.);
- get as much rest as possible;
- Eat foods high in fiber and plenty of fruits and vegetables, while limiting the amount of fat in your diet.
In the first days of an acute respiratory infection or acute respiratory viral infection, appetite usually decreases. This is normal and should pass soon. Don't force yourself or your child to eat against their will. In addition to these measures, there are various medications, which relieve symptoms and help you cope with a cold faster.
Drug treatment of colds (ARI, ARVI)
The main medications used to treat symptoms of colds are:
- painkillers such as paracetamol or ibuprofen help with high fever and pain;
- decongestants are vasoconstrictors that help with a runny nose;
- combination cold remedies;
- antiviral drugs.
All of these products can be bought at the pharmacy without a prescription. They are generally safe for older children and adults. For small children, pregnant women, sick people chronic diseases There are a number of restrictions on taking cold medicines, which should be discussed with your doctor. In any case, before purchasing and taking a medicine, always carefully read the manufacturer’s instructions, recommendations on the treatment regimen and dosage of the drug. More information on drug treatment ARI (ARVI) is contained below.
Painkillers: Paracetamol and ibuprofen reduce body temperature and also reduce pain. Aspirin has a similar effect, but it should not be given to children under 16 years of age.
If your child has a cold, you can find paracetamol or ibuprofen in a special dosage form for children (usually in the form of a suspension). Always follow the instructions to ensure correct dosage. Taking these drugs together for colds in children is usually not necessary and should be avoided.
It must be remembered that paracetamol and ibuprofen are often included in combined agents from a cold. Therefore, if you want to take such a medicine and, at the same time, an anesthetic or antipyretic, look at the composition of the drug (on the package, in the instructions) or consult a doctor to avoid an overdose.
For pregnant women, paracetamol is the drug of choice for fever and pain.
Decongestants are vasoconstrictors that are usually used as drops or a nasal spray. They relieve swelling from the nasal mucosa and sinuses, thereby facilitating breathing and improving the flow of sinus contents from the nose (to prevent sinusitis). However, nasal decongestants are only effective for 5-7 days. If you use them longer, the symptoms of a runny nose may only get worse.
Vasoconstrictors have their own contraindications and are not suitable for everyone. You need to be especially careful when using nasal drops in young children. In this category of patients with acute respiratory infections, treatment should only be prescribed by a doctor.
Antiviral drugs- able in various ways prevent viruses from multiplying and penetrating into cells. If you start taking these drugs in the first hours of the disease, you may be able to shorten the period of fever and poor health, and in severe cases viral infection- prevent complications. However, with a mild cold, it is not always possible to feel the effect of these drugs; in addition, the body copes with the infection on its own. Therefore, the prescription of drugs from this group for acute respiratory infections and acute respiratory viral infections occurs at the discretion of the doctor.
Additional remedies for colds
Relief from a sore throat and runny nose can be brought by frequent gargling with warm salt water, soda and sucking on lozenges (with menthol, essential oils, antiseptics and antibiotics). To improve nasal breathing in infants you can use drops of saline solution.
According to some data, vitamins and nutritional supplements with zinc and vitamin C can relieve cold symptoms and ease the course of acute respiratory infections (ARVI), especially at the onset of the disease, but there is no convincing evidence for this opinion yet.
- antihistamines;
- cough expectorants - however, your doctor may prescribe sputum thinners (mucolytics) for coughs with thick, difficult-to-clear phlegm or antitussives for dry, hacking coughs;
- antibiotics - effective only against bacteria, can be prescribed by a doctor according to strict indications;
- alternative medicines such as echinacea or Chinese herbal remedies.
Complications of acute respiratory infections (ARVI)
Colds, with the exception of influenza, rarely cause complications, however, sometimes the infection spreads to the organs chest, ears or sinuses.
Sinusitis- infection of the paranasal sinuses - sinuses filled with air. This complication occurs in 1 in 50 adults and older children with cold symptoms. Manifestations of sinusitis include:
- pain or increased sensitivity around the nose, eyes, forehead;
- nasal congestion and discharge from the nasal passages;
- temperature up to 38°C and above.
Typically, sinusitis resolves spontaneously, but if symptoms are severe or do not go away after a week, consult your doctor.
Otitis media- Middle ear infection - develops in approximately one in five children aged 1-5 years with cold symptoms. Signs of ear damage are:
- severe pain in the ear;
- temperature up to 38°C and above;
- flu-like symptoms such as severe general malaise, nausea and vomiting.
Otitis media usually does not require special treatment and goes away within a few days. If your child shows symptoms of otitis media again, you will need to see a doctor.
Chest infection— bronchitis and pneumonia can occur after a cold, since during this period the body’s immune defense is temporarily weakened. The development of these complications can usually be judged by the appearance of a persistent cough with sputum and shortness of breath (difficulty and rapid breathing). Mild infections clear up on their own within a few weeks, but you should see a doctor if:
- have a strong cough;
- holds on heat;
- periods of disorientation or confusion appear;
- there is acute pain in the chest;
- hemoptysis is observed;
- symptoms last more than 3 weeks.
These signs indicate the development of a bacterial infection that needs to be treated with antibiotics.
A child has a cold
Young children often get colds because their immune systems are still developing and cannot fully resist infections. Of course, acute respiratory infections and acute respiratory viral infections in a child cause a lot of concern for parents, however, fortunately, in most cases these infections go away without consequences within 10-14 days. Below are answers to the most FAQ that worry parents of sick children.
ARI in a child: how serious is it?
Children usually recover well from a cold, although they are at risk for developing complications such as ear infections. Very rarely, problems such as pneumonia (pneumonia) may develop. Therefore, it is extremely important to keep an eye on your sick child until he feels well.
Is there a difference in the course of colds in children and adults?
Children, as a rule, suffer from acute respiratory infections (ARVI) more often than adults. If an adult on average gets colds 2-4 times a year, children sometimes manage to get respiratory infections 8-12 times.
Cold symptoms are similar for people of all ages. This includes a runny nose, sneezing and high fever. In most cases, children recover without outside help, although it takes longer than in adults. Sometimes it may seem that the child already has a very cold long time and cannot cope with the disease in any way, although in fact it turns out that mild acute respiratory infections replace one another, and between them there are short periods of recovery.
When should you see a doctor if your child has a cold?
Contact your doctor if:
- a child under 3 months of age has a fever of up to 38°C, in a child under 6 months of age - up to 39°C;
- cold symptoms last longer than 3 weeks;
- the child’s condition worsens;
- the child complains of chest pain or coughing up blood - this may be a sign of a bacterial infection and requires treatment with antibiotics;
- the child has difficulty breathing - seek medical help immediately;
- worries about ear pain - babies with ear pain often rub their ears and seem irritated;
- the child has a severe or prolonged sore throat;
- other alarming symptoms develop.
Why didn’t the doctor prescribe antibiotics for acute respiratory infections?
Antibiotics are indicated to treat bacterial infections. Colds in most cases are associated with viral infection and therefore cannot be treated with antibiotics. Overuse of antibacterial drugs can lead to the development of antibiotic resistance, where any subsequent bacterial infection may become more severe and difficult to treat.
Antibiotics for ARVI are prescribed only when certain complications develop.
How to help a child with a cold?
To help a child who is sick with acute respiratory infections (ARVI), follow our advice:
- Provide your child with rest, quiet and make sure he drinks enough fluids; You can use water or warm drinks for drinking - they are soothing;
- if the nose is stuffy, raise the head end of the bed, placing a stack of books or bricks under the legs, you can give the child a high pillow - this advice is not suitable for children under one year old;
- to relieve fever or pain, give paracetamol or ibuprofen as directed; never give aspirin to children under 16 years of age;
- Warm, moist air helps to ease breathing when you have a runny nose; use a humidifier or take your child to the bathroom and turn on a hot shower to saturate the air with moisture;
- Ventilate the child’s room often, maintain a comfortable temperature in it, avoid overheating, for example, cover the patient with a light sheet.
Which doctor should I see if I have a cold?
Using the NaPopravka service, you can find a good therapist, family doctor or pediatrician (for a child), and also choose a clinic where you can call a doctor at home.
Colds and colds-infectious diseases
Colds and cold-infectious diseases in Russia are among the most common, although the specific resistance of the human body to low temperatures is quite high 20. In this case, we should talk about the distortion of the perfect mechanisms of thermoregulation formed in evolution in modern humans.
Humans are warm-blooded organisms, i.e. having a constant body temperature. This property is provided by a complex system thermoregulation, which, if there is a danger of overheating, reduces heat production and increases its output, and if there is a danger of hypothermia, it activates heat production while limiting its output. Thermoregulation in humans works quite reliably, provided that the environment supports its active state, i.e. allows the body to remain at a constant temperature of about 36 – 37°C. Such conditions correspond to an ambient temperature of 16 – 18°C: at a lower temperature the body is at risk of hypothermia, and at a higher temperature – overheating. However, a person is most often in an ambient temperature that threatens him with overheating, which is largely facilitated by warm clothes and high room temperature. In this case, the mechanisms for maintaining normal body temperature at low ambient temperatures in most people turn out to be detrained, which leads to the development of colds and colds and infectious diseases.
Etiology. The main causes and conditions for the occurrence of colds and colds and infectious diseases are the following.
1. Decreased immunity associated with hypothermia, weakening of the body, physical or mental fatigue, abuse of bad habits, chronic or long-term anxiety, etc.
2. Insufficient physical activity eliminates the active maintenance of normal body temperature with the threat of hypothermia, the main significance of which is played by the increased tone of skeletal muscles. Under these conditions, a person has to resort to artificial conditions (warm clothes, comfortable room temperature, etc.), which disrupts thermoregulation mechanisms.
3. Slagging in the body in case of hypothermia, it makes the respiratory tract almost the main channel for the elimination of waste substances entering the body or formed in it as a result of metabolic processes. The swelling and looseness of the respiratory tract that occurs under these conditions make their mucous membrane easily permeable to pathogenic viruses.
4. Sudden temperature fluctuations, especially during a rapid transition from an environment with high temperatures to an environment with low temperatures.
Despite the importance of these risk factors for colds and colds and infectious diseases, the main one is still a decrease in immunity and the body’s resistance to low temperatures. The most effective means of training them is hardening.
The importance of hardening lies in its diverse effects, the main of which are:
1) increased immune activity and resistance to infection;
2) increasing resistance to a decrease in body temperature;
3) increase in heat production when exposed to low temperatures;
4) easier tolerability in terms of severity and duration of emerging colds and colds-infectious diseases.
Although all colds and colds and infectious diseases have certain common characteristics, there are also serious differences between them that should be taken into account for their prevention and therapy. These differences are associated both with the predominant cause that caused the corresponding disorder and with the symptoms manifested in this case.
Classification. Based on an analysis of etiology and pathogenesis, the whole variety of diseases caused by hypothermia can be classified into two main groups - colds and colds-infectious diseases.
Most common colds are rhinitis(runny nose), laryngitis(inflammation of the larynx), pharyngitis(inflammation of the trachea), bronchitis(inflammation of the bronchi).
The main reasons for the occurrence of colds are slagging in the body and sharp changes temperatures
With adequate sweating, a significant portion of substances entering the body that do not have a natural origin (with food, water, air, as a result of bad habits, etc.), as well as substances formed as a result of vital activity, are removed with sweat. At low ambient temperatures, when sweating stops, the respiratory system takes over the function of cleaning the body: the resulting swelling of the respiratory tract is defensive reaction, aimed at removal from the body along with secretions harmful substances. However, if such swelling persists for a relatively long time, the mucous membrane of the respiratory tract becomes easily permeable to infectious microorganisms, and a cold-infectious disease develops.
Another factor that provokes a cold is sudden changes in external temperatures. When a person is at an ambient temperature that threatens him with overheating, sweating is compensatory activated: when 1 ml of sweat evaporates, the body loses up to 0.56 kcal of heat, which allows maintaining normal body temperature. Human thermoregulation is relatively inert, therefore, when leaving a warm room into frosty air, it takes at least five to seven minutes to adjust it from the heat transfer mode, which prevents overheating of the body, to the mode, which protects it from hypothermia during low temperatures. If the transition from heat to cold turns out to be much shorter (as is most often the case), then even in the cold the body continues to give off heat. This makes clear the danger of a sweaty person being in the cold - intense heat loss through sweating causes hypothermia of the body. The situation is aggravated by the fact that, already in the frosty air, a person in warm and heavy clothes moves little, and the cold air entering his lungs causes disturbances in their activity.
The amount of slagging in the body decreases when the intake of waste-forming substances into the body is limited or when the removal of toxins from the body is activated. Both of these effects are achieved by switching to eating predominantly raw plant foods, which contain a significant amount natural ingredients and, in addition, stimulate the immune system. During periods dangerous for the occurrence of colds, you should limit the consumption of table salt, which, by retaining water in the body 21 and limiting sweating, makes it difficult to remove waste substances from the body. At the same time, giving up salt activates the breakdown of fats, which are called “sinks of waste” in the body, and the water formed during the breakdown is excreted along with the waste.
Cleansing the body of toxins that have entered or formed in it is possible in several ways: drinking plenty of fluids (if there are no contraindications from the cardiovascular system, kidneys or carbohydrate metabolism), a bath (preferably a dry air bath, where not only the body is cleansed of toxins, but also caused by high temperature kills viruses), etc.
In order to prevent the negative impact of sudden temperature changes in the development of colds, it is important to maintain the room temperature at a level of up to 22 – 24°C. Above the specified temperature, active sweating begins in the body, preventing overheating. Sweating increases, and in widely practiced attempts, you should stock up on warmth (such as hot drinks) before going out into the cold.
Colds and infectious diseases(flu, ARVI, sore throat, etc.) can occur at any time of the year, since the main reason for their development is a decrease in immunity associated with many circumstances of an unhealthy lifestyle: overwork, bad habits, strong or prolonged exposure to stress factors, etc. However, They spread more often and wider in the cold season due to the fact that during hypothermia:
– immune activity decreases, and the body is unable to successfully resist infection;
– swollen and loose mucous membrane of the respiratory tract becomes easily permeable to pathogens.
Although both colds and flu (as a typical cold-infectious disease) are caused by viruses, there are significant differences between them, which is manifested in the symptoms of their course (Table 10).
Table 10
Symptoms of colds and flu
From the table above it can be seen that colds most often only affect the respiratory system: nasopharynx, throat, upper respiratory tract. In infectious diseases, the whole body reacts in the form of high fever, chills and more serious symptoms. Therefore, the latter almost always occur in a more severe form than a cold. A characteristic feature that distinguishes them from a cold is a sudden onset with high fever and chills. With conventional methods and means of treatment, a cold goes away in two to five days, and complete restoration of the body’s vital functions takes one to one and a half weeks. The active phase of colds and infectious diseases usually lasts about a week, but residual effects - weakness, loss of strength, muscle pain and others - can persist for another two to three weeks.
Currently, in the treatment of colds and colds and infectious diseases, rest and pharmacology are considered the main means. Since the causes of these diseases are different (hypothermia and slagging of the body in the first case and decreased immunity and infection in the second, although the factors indicated for colds also have a certain significance in reducing immunity), then human behavior and approaches to their treatment should be different .
At cold Efforts must be made to rid the body of toxins as quickly as possible. There are several ways you can help in this case:
By abstaining from food (if there are no contraindications) with plenty of fluids or, according to at least, switching to eating only raw plant foods;
Complete refusal of table salt;
For a runny nose, good results are achieved by those products that clean (but do not dry out) the nasal mucosa and thereby improve the conditions for the discharge of secretions (rinsing the nose with salt water, instilling solutions prepared from honey and juices of onions, carrots, beets, washing with soapy water, etc. .d.).
When you have a runny nose, it is better to refrain from using those medications that, by drying out the mucous membrane of the nasal passages, reduce nasal discharge and thereby make it difficult to cleanse the body of toxins. In this case, the swelling descends to the lower parts of the respiratory tract - the larynx and trachea, which leads to coughing. The cough itself is an adaptive reaction aimed not only at cleansing the body of toxins, but also at clearing the respiratory tract from infectious agents, mechanical and other harmful substances. Therefore, a cough accompanied by the discharge of sputum is beneficial. With such a cough, it is also inappropriate to use drugs that cause drying of the mucous membrane of the respiratory tract. On the contrary, a dry cough is unproductive, as it does not help clean the respiratory system. It is softened by drinking plenty of water (together with honey, horseradish juice, mustard), gargling (with solutions of salt, soda, honey, etc.). Suppressing cough with medications also makes it difficult to cleanse the body of waste substances - in this case, the swelling descends to even lower areas of the respiratory apparatus.
Whenever colds and infectious diseases human behavior should be different, because in these conditions the body primarily directs its efforts to fight against infection. Therefore, with the development of these diseases, a feeling of weakness, muscle pain and other symptoms arise, leading to a limitation in energy expenditure on aspects of life other than immunity. This is also associated with a decrease in the patient’s appetite, but in relation to food, first of all, one should analyze the patient’s own feelings: one should not force oneself to eat, but if a clear feeling of appetite arises, it must be quenched using natural, raw plant products.
Another protective reaction of the body directed against the causative agent of an infectious disease is fever – increase in body temperature. With it, the reproduction of viruses and their vital functions are hampered, and the effect of the body’s defenses on them is more effective. Therefore, taking antipyretics from the very beginning of the disease only increases its duration. However, if the temperature rises above 39° or the high temperature lasts more than three days, you should definitely follow your doctor’s recommendations regarding the use of pharmacology.
Exercise therapy for colds and colds and infectious diseases, Like treatment, it has its own characteristics.
Beneficial effect motor activity in the prevention and treatment of colds and colds and infectious diseases is determined by the significant role that movement plays in maintaining a stable body temperature. In this regard, of particular importance is skeletal muscle tone, which increases at low ambient temperatures and decreases with warming. For example, when trembling, the body's heat production can increase more than three times, and during strenuous physical work - even ten times or more. In this case, at the first signs of a beginning decrease in body temperature, active physical activity contributes to the production of additional heat, which prevents the beginning decrease in temperature. Therefore, it is especially important to emphasize the importance of light clothing, which forces a person to actively move at low ambient temperatures. Practice shows - As long as a person moves, he is not in danger of catching a cold.
Increased breathing during muscle work helps good ventilation with the elimination of stagnation and the active removal of microorganisms and foreign substances that have entered here.
During prolonged intense muscular work, heat production is so intense that even in cold air conditions an increase in body temperature can occur. This causes a compensatory increase in sweat production, which provides removal of toxins from the body .
It has been proven that moderate physical activity helps increasing the level of immunity person. It is especially important that both cellular and tissue immunity are stimulated 22 .
Physical activity for colds and colds-infectious diseases solves the following: tasks:
1) activation of the immune system;
2) stimulation of sweating as an effective way to cleanse the body of toxins;
3) production of additional heat by the body.
Prevention colds should consist of eliminating (or at least reducing the influence of) both factors that provoke its development - sudden changes in external temperatures and excessive accumulation of waste substances in the body. This condition also determines the selection of exercise therapy products.
To prevent the influence of sudden changes in external temperatures, various means and techniques can be used. Some of them represent systemic forms that are regularly used in human life. First of all, this is systematic hardening, which increases the body's resistance to low temperatures. Another effective and everyday remedy is to maintain in the cold seasons in the room a temperature (below 20 - 22°C) that does not yet activate sweating, which, on the one hand, eliminates the subsequent intense transfer of heat by the body when switching to cold, and on the other hand - in itself is a form of hardening for the body.
Other forms and means of prevention and treatment of colds can be considered as urgent measures taken at a time. They should be aimed at forcing the body to stop sweating and, therefore, give off heat in the cold. To do this, for example, before leaving a warm room into cold air, you need to carry out a kind of “cold warm-up” - put your hands under running cold water for 10-15 seconds, gargle with cool (but not ice-cold!) water, etc.
A massage of the neck and throat, especially in the area of the tonsils, gives a good effect before going out into the cold air.
If a person nevertheless finds himself hot in the cold, he must move, gradually reducing the intensity of movement until sweating stops completely. The necessary effect is achieved by the fact that both hands are simultaneously or alternately exposed to cold.
As for preventing excessive accumulation of slag products in the body, in addition to the corresponding restrictions in Everyday life(in nutrition, bad habits etc.) the bathhouse is important. This is due to intense sweating that occurs during vaping, due to which many harmful substances that have entered or formed in it are removed from the body.
For treatment already existing colds, the first sign of which is a runny nose, should to live an active lifestyle, aimed at cleansing the body and maintaining thermoregulation. This means that a person needs not only to maintain the usual mode of activity (including the continuation of work or educational activities, physical activity 23, etc.), but also to activate sweating using, for example, a sauna or moderate physical activity (in the absence of contraindications) .
For prevention and treatment of colds and infectious diseases The forms and means of exercise therapy are somewhat different.
IN prevention For these diseases, strengthening the immune system should be of primary importance. Most effective means This is what hardening is for. In addition to generally accepted means, the simplest techniques that are available in everyday behavior can be used. In particular, these may be:
Light clothing for the season;
Moderately cool fresh air in the room;
Washing only with cold water;
Local hardening of the legs;
Walking barefoot - at home and outdoors, if possible with a sharp temperature change;
Contrast shower, cold douches, etc.
The high effectiveness of stimulating the immune system using certain techniques has been proven acupressure. In particular, the method proposed by A.A. has become widespread. Umanskaya. This method applies acupressure to nine single or biologically symmetrical active points, that are " entrance gate» infections: upper respiratory tract, eyes, mouth, nose, etc. (Fig. 33). It is important that this not only stimulates the immune system, but also has a normalizing effect on the activity of various organs and functional systems.
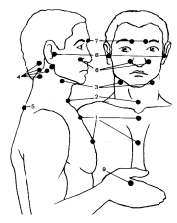
Rice. 33. The influence of acupressure according to A.A. Umanskaya on organs and systems
1 – sternum (normalization of the state of the cardiovascular system, bone marrow, esophagus, trachea, bronchi, lungs); 2 – jugular notch (immunity, thymus); 3 – paired sinocarotid glomeruli ( chemical composition blood, homeostasis, metabolism); 4 – paired mastoid processes (brain); 5 – spinous process of the seventh cervical vertebra (compensation for the influence of the external environment); 6 – paired places at the base of the wings of the nose (production of biologically active substances, mucous membrane of the nasal passages); 7 – paired exit points of the trigeminal nerve (eliminates headaches and eye pain); 8 – paired places at the tragus of the ear (cerebral cortex and vestibular apparatus); 9 – paired places on the back of the hand between the first and second fingers (eliminates headaches and runny nose)
In the prodromal period, at the first signs of malaise, acupressure is performed in the same sequence every 40 - 60 minutes. In addition, massage of the reflexogenic and acupressure zones of the auricle - right for right-handers and left for left-handers - also gives a good effect at this time. Massage should be done exactly in the sequence indicated in Fig. 34. Zone 4 especially requires attention (improves trophic processes in the lymphoid pharyngeal ring and the immunological activity of the body). The effect of the massage can be prolonged by applying 5 anti-inflammatory and warming rubs to the indicated points (analgesic and anti-inflammatory effects).
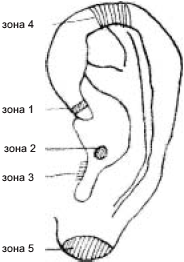
Rice. 34. Acupressure of the auricle for colds and infectious diseases
Colds and infectious diseases are an acute reaction of the body to infection, and therefore require the mobilization of a significant part of the reserve capacity. In this regard, active forms of therapy recommended for colds cannot be used for these diseases, and bed rest is recommended for patients. For the same reason, physical activity should be sharply limited. You cannot resort to the help of a bath, which in itself is a significant burden for the body.
Colds and infectious diseases are most often accompanied by an increase in body temperature (fever), which is a protective reaction. Therefore, forcibly reducing body temperature using pharmacology only complicates and prolongs the course of the disease. On the other hand, stimulation of heat production by cold influences (wet wraps, cold shower etc.) gives an exceptionally quick – within several hours or even several tens of minutes – healing effect.
Method of using a cold shower at elevated body temperature. When body temperature rises, to normalize it, you need to use a cold shower as follows.
The water in the tap should be as cold as possible, only the body should be doused, and the duration of the dousing itself for an unseasoned person should not exceed 15 - 20 seconds (in no case should chills be allowed); After this, the body should be vigorously rubbed, dressed warmly and went to bed. Drinking plenty of warm drinks will also help. After 15 - 20 minutes, you should definitely measure your body temperature and, if it has not at least increased, perform the entire cold shower procedure again. Usually three to four repetitions of a cold shower are enough to normalize the temperature. If after the first procedure the temperature has increased (even slightly), further douches should not be carried out, because, most likely, the cause of the increase is of a non-infectious nature.
Bronchitis – infectious-inflammatory disease of the bronchi.
Predisposing factors for its development are: hypothermia, inhalation of toxic, allergic substances, exposure to professional conditions, etc. From everyday living conditions, dry indoor air can have a certain significance in the occurrence of bronchitis (as happens in the cold season due to central heating): entering the respiratory tract, it dries out the bronchial mucosa, depriving it of bactericidal activity and provoking a dry (“barking”) cough, which irritates the bronchi.
There are acute and chronic bronchitis.
Acute bronchitis. Etiology this disease is most often associated with pathogenic staphylococci, pneumococci, viruses; Air pollution also plays a certain role. As for chronic bronchitis, most often it develops as a result of long-term, untreated acute breathing disorders.
Pathogenesis. The pathological process affects all layers of the bronchi, accompanied by swelling, disruption of their blood and lymph supply, atrophy and proliferation of connective tissue. The inflammatory process leads to disruption of the functions of the bronchial tree - drainage, barrier, etc., as a result of which pathological infected contents accumulate in the bronchi, promoting sensitization and the development of deformities.
In the clinic of acute bronchitis, swelling and narrowing of the lumen of the bronchi, a feeling of chest compression, and shortness of breath are noted. The cough is prolonged, with scanty sputum. The temperature is low. Breathing is weakened. The course of the disease is favorable, but in case of improper treatment, acute bronchitis can become chronic. With frequent repetitions, bronchosclerosis occurs with the involvement of lung tissue. The clinical picture of chronic bronchitis during periods of exacerbation is characterized by low-grade fever, malaise, cough with sputum, and increased fatigue.
Treatment chronic bronchitis is carried out for a long time, taking into account the fact that its outcome can be such serious diseases as chronic pneumonia, bronchiectasis, bronchial asthma, etc. The patient is prescribed a medical and protective regime adequate to his condition with maximum use of fresh air and walks; Antibacterial therapy, vitamin therapy are carried out, physiotherapy and exercise therapy are widely used.
Therapeutic physical education is prescribed during all periods of prevention and treatment of chronic bronchitis. Physical exercises that involve the muscles of the chest and upper limbs provide improved lymph and blood supply to the bronchopulmonary system due to anatomical, functional and motor-visceral relationships.
To prevent bronchitis, the main types of physical activity can be walking, running, skiing and other exercises that train the respiratory system, ensure active ventilation of the lungs and eliminate congestion in them. However, without accompanying hardening of the body, these measures can only give partial results.
In the treatment of bronchitis, physiological prerequisites should be created to reduce and eliminate inflammatory changes in the bronchi and prevent their hardening. For chronic bronchitis, drainage breathing exercises are used as special exercises to promote the evacuation of pathological contents of the bronchi, thereby improving and normalizing the corresponding functions of the bronchial tree. The anti-inflammatory, trophic effect of special breathing exercises is enhanced when combined with general developmental ones, which have a stimulating effect on blood circulation and breathing.
The leading role in exercise therapy is played by means that increase the body’s nonspecific resistance and thereby prevent the occurrence of colds that provoke exacerbation of bronchitis. Physical activity, which increases as adaptation to it develops, helps to increase not only the general, but also the local resistance of the bronchial tree. However, in the acute period of bronchitis, these measures should be used with caution, so they are fully consistent with those noted for colds in general.
After the end of the acute period of the disease, hardening becomes of utmost importance, however, serious attention should be paid to the prevention of any hypothermia, therefore, before going out into the cold air, appropriate preparation (for example, “cold warm-up”) and clothing are necessary.
Massage for bronchitis is carried out with the patient sitting or lying on his stomach. Massage the back from the lower back to the neck with targeted effects on the spinous processes (especially pay attention to the point of the process of the seventh cervical vertebra - da-zhui). When massaging the anterior surface of the chest, carefully massage the intercostal spaces and perform an indirect massage of the lungs: soft push-like pressure on different zones chest, squeezing the chest with the palms from the front, from the sides, tapping the chest. Finish the massage with breathing exercises with an emphasis on deep exhalation (draining effect).
The organization of exercise therapy is determined by the treatment tactics for patients suffering from chronic bronchitis. In a clinic setting, classes are held for them in classrooms. Children attending school during periods of remission engage in physical education in the preparatory group; transfer to the main group and passing any standards are carried out no earlier than complete recovery and removal of the child from the dispensary register. In case of exacerbation of chronic bronchitis and hospitalization, the method of exercise therapy is based on the motor mode.
Pneumonia, or pneumonia – acute or chronic disease characterized by inflammation of the parenchyma and (or) interstitial tissue of the lungs.
Pneumonia – quite frequent illness, especially in childhood and older ages. This is due to the anatomical and physiological characteristics of people of these groups, which determine the low reserve capabilities of the respiratory apparatus, the ease of bronchial obstruction, the tendency to edema, atelectatic processes, etc.
Most pneumonias are divided into lobar (lobar), when the entire or significant part of the lung lobe is affected by the inflammatory process, and focal (lobular), in which individual areas (lobules) of the lung are involved in the pathological process. Focal pneumonia is most often a complication of inflammation of the upper respiratory tract and bronchi in patients with congestive lungs, severe, debilitating diseases in the postoperative period (especially in the elderly).
Etiology pneumonia – viral-microbial, mixed. Among bacterial pathogens, the leading role is played by staphylococci, streptococci, pneumococci, and Escherichia coli; viruses – adenoviruses, influenza, respiratory syncytial. Conditions that provoke the pathogenic influence of microorganisms are either hypothermia or congestion in the lungs, characteristic of hypokinesia and long-term maintenance of a forced posture with a decrease in pulmonary ventilation (for example, in conditions of skeletal traction during a spinal fracture). Quite often, pneumonia develops as a result of chronic bronchitis, when inflammation spreads down the bronchial tree all the way to the lung tissue.
Pathogenesis. The most important aspects of the pathogenesis of pneumonia are the spread of infection, the development of inflammatory changes, impaired respiratory function and disorders of autonomic functions. Due to edema and swelling of the mucous membrane, as well as the accumulation of secretions in the bronchi, which leads to deterioration of bronchial patency, part of the alveoli is excluded from ventilation and gas exchange. In this case, the diffusion of gases through the damaged alveolar wall is disrupted. In addition, there is a violation of the regulation of breathing with discoordination of the respiratory muscles and uneven ventilation in different lobes and parts of the lungs.
All of these changes quickly lead to significant changes in the patient’s body as a whole, in particular to disturbances in the central nervous system, changing its functional state with a predominance of inhibitory processes. Dysfunction of the autonomic nervous system; The more pronounced the respiratory failure and signs of intoxication, the more significant disturbances are found in the cardiovascular system of a patient with pneumonia. Very frequent disorders are detected in the digestive, excretory, and endocrine systems. Metabolic disorders (protein, carbohydrate, fat) and the development of metabolic or respiratory-metabolic acidosis are typical. Consequently, pneumonia is a severe general disease of the body.
Clinic acute pneumonia is characterized by the following symptoms: fever, chills; pain when breathing on the side of the affected lung (especially if pleurisy occurs), which intensifies with coughing, initially dry, later with viscous sputum; increase in ESR.
Treatment pneumonia is complex in nature against the background of a medical and protective regime. In the acute period, bed rest is prescribed, which lasts for at least three days after the temperature drops and the clinical signs of respiratory failure disappear. Particular attention is paid to antibacterial therapy. Under the influence of the treatment, the temperature decreases, the patient's condition improves, the cough becomes moist, sputum is released, signs of respiratory failure decrease, changes in the heart, liver, and kidneys disappear, the gas composition of the blood improves and gradually normalizes. All these signs allow the patient to be transferred to the ward. Finally, when pneumonia passes into the period of residual effects and recovery, a general hospital regime is prescribed. However, the massive damage to the respiratory system and many internal organs in lobar pneumonia requires long-term treatment using the entire range of means to achieve a successful outcome and prevent complications.
Physiotherapy in case of pneumonia, it has multifaceted effects on the body, providing a beneficial effect of functional therapy.
First of all, it should be noted the increase under the influence physical exercise flow of exhaled air, which ensures the removal of secretions from the respiratory tract, along with which they are freed from pathogens of pneumonia. The restoration of bronchial patency is also facilitated by a reduction in swelling of the bronchial mucosa. Of no small importance are the elimination of congestion in the lungs, the restoration of the relationship between pulmonary ventilation and pulmonary blood flow disrupted by the pathological process, and the improvement of the diffusion of gases in the lungs and the transport of gases in the blood. The use of physical exercises deepens and slows breathing and normalizes its rhythm. Restructuring respiratory movements not only increases the efficiency of breathing, but also reduces unnecessary energy consumption for the respiratory act.
Exercise therapy for pneumonia is prescribed from the first days of the disease. Her main tasks are:
1) compensation of respiratory failure;
2) reduction of congestion in the lungs;
3) stimulation of the body's defenses to fight the disease.
In the first period, with bed rest, contraindications Exercise therapy includes exercises with holding your breath while inhaling, with hyperventilation, and also performed with high intensity. The main means of exercise therapy during this period are breathing exercises and gymnastic exercises, as well as massage.
Breathing exercises drainage type and with an emphasis on prolonged exhalation help eliminate secretions from the respiratory tract and facilitate the act of breathing itself. They should be performed at a slow pace, without resistance to breathing or forcing it. If there are signs of acute phenomena subsiding, breathing exercises are combined with simple gymnastic exercises for medium muscle groups (especially the shoulder girdle), performed at a slow pace and from lighter starting positions on the back, on the side, with frequent changes.
Both in combination with physical exercises and independently in the first period, massage techniques (mainly stroking and partly rubbing) of the torso and limbs can be used. When massaging the chest, attention is paid to coordinating the pressure on it with the exhalation phase, which creates the prerequisites for removing secretions from the respiratory tract and eliminating congestion in the lungs.
With a duration of active exercises of 10 - 12 minutes and subsequent massage of 8 - 10 minutes, the frequency of use of this complex should be at least six to eight times during the day.
In satisfactory condition, normal temperature and compensated respiratory failure or its absence, the patient is transferred to the ward mode. In this period of the disease - the period of reverse development of pneumonia - main tasks of exercise therapy are:
1) improvement of external respiration indicators;
2) acceleration of resorption of inflammatory infiltrates in the lung tissue;
3) general strengthening of the body and adaptation of the patient to physical activity within the ward regime.
Among the means of exercise therapy, the most important are still breathing exercises, in which resistance breathing is increasingly emphasized. Their combination with general developmental gymnastic exercises is performed from a variety of starting positions, promoting the activation of breathing in the affected segment and lobe of the lung and the drainage of infiltrate from them. Morning hygienic gymnastics, the complex of which includes not only special, but also general strengthening exercises, becomes an obligatory element of the motor regime in this period.
In the second half of the ward regime, the patient is introduced to walks, and then to dosed walking, performed in an aerobic mode with a gradual increase in the time of its implementation.
The total time of daytime physical activity of the patient by the end of the ward should be at least one and a half to two hours.
When transferring the patient to general mode(recovery period), when he still has residual effects, tasks of exercise therapy are:
1) complete restoration and normalization of external respiration function and an increase in its reserves;
2) adaptation of the patient to the stresses of the domestic and professional regime;
3) increasing the nonspecific resistance of the child’s body.
The leading role in the method of exercise therapy during the recovery period is played by exercises of a general strengthening and general developmental nature for all muscle groups from various starting positions. Among them, a special place is occupied by long-term low-intensity cyclic exercises aimed at strengthening the respiratory and cardiovascular systems (walking, running, swimming, skiing, etc.), as well as dosed hardening, which provides immunity training. The patient’s attention is still drawn to performing breathing exercises that help consolidate his skills correct breathing(in particular, the full and effective use of thoracic and abdominal types of breathing and the combination of phases of the respiratory act), and the elimination of residual effects of the inflammatory process in the bronchi.
The duration of exercise therapy sessions reaches 35–40 minutes with one or two sessions per day.
The technique and methodology of massage for pneumonia is not fundamentally different from those for bronchitis, however, you should carefully massage (for lobar pneumonia) the area where the infiltrate accumulates.
Tonsillitis and tonsillitis - respectively chronic and acute inflammation palatine tonsils. These diseases are often the cause of the development of many diseases of the heart, joints, kidneys, etc. Such serious consequences are due to the fact that the palatine tonsils (or tonsils) play an important role in providing immunity, i.e. their condition significantly affects the overall health of a person.
Etiology. The development of tonsillitis is largely facilitated by poor conditions of professional activity and everyday life (dustiness, gas pollution in the premises), non-compliance with the requirements of oral hygiene and foci of purulent infection in the oral cavity and nose: caries teeth, difficulty in nasal breathing, etc. Bad addictions are also of undoubted importance, including particularly smoking.
Pathogenesis. The chronic course of inflammation is accompanied by the destruction of tonsil tissue and the entry into the blood of the products of their decay and the vital activity of microorganisms. These products can cause a chronic inflammatory disease in organs rich in connective tissue - rheumatism, which is difficult to treat. The heart (rheumatic carditis) and joints (rheumatoid arthritis) are most often affected by rheumatism.
As the disease progresses, the tonsils become loose and increase in size; infectious microorganisms that cause inflammation easily multiply on them. Under unfavorable conditions (especially during hypothermia), inflammation of the tonsils easily turns into an acute form - sore throat. The disease is accompanied by severe general reactions of the body and an increase in temperature. Depending on the severity and form of angina, its active phase can last from seven days to a month.
The main means of preventing tonsillitis and sore throat is to comply with the requirements of oral hygiene, regular gargling with decoctions of anti-inflammatory plants, abstaining from bad habits, etc. When staying in frosty air, you need to worry about warmly covering the front surface of the neck, since it is behind its thin wall that the tonsils. Sudden temperature changes are also dangerous for them (for example, when a hot person drinks ice water or eats ice cream).
Exercise therapy in the prevention and treatment of tonsillitis and tonsillitis turns out to be quite effective. The main condition for this is to increase blood flow to the tonsils. To do this, they should be regularly (especially before going out into the frosty air) massaged through the surface of the skin under the lower jaw or use the “lion pose”, when the root of the tongue performs a kind of massage of the tonsils.
In the presence of tonsillitis and in the initial stage of development of sore throat, a good result is achieved by performing a complex that includes the “lion pose”, massaging the tonsils and gargling with a solution of table salt (or soda) and iodine. In the presence of tonsillitis, this procedure should be performed at least twice daily, and if a sore throat occurs, every 15 to 20 minutes. In this case, the duration of a sore throat is reduced many times over, and with the active use of this complex in the initial phase of development of a sore throat, sometimes the inflammatory phenomena disappear within one to one and a half hours.
